- Department of Neurosurgery, Hospital de Clínicas José de San Martín, Facultad de Medicina, Universidad de Buenos Aires, Buenos Aires, Argentina
- Department of Psychiatry and Behavioral Sciences, Stanford University, Stanford, California, United States,
- Department of Radiology, Hospital de Clínicas José de San Martín, Facultad de Medicina, Universidad de Buenos Aires, Buenos Aires, Argentina
Correspondence Address:
Pablo Raul Devoto, Department of Neurosurgery, Hospital de Clínicas José de San Martín, Facultad de Medicina, Universidad de Buenos Aires, Buenos Aires, Argentina.
DOI:10.25259/SNI_356_2024
Copyright: © 2024 Surgical Neurology International This is an open-access article distributed under the terms of the Creative Commons Attribution-Non Commercial-Share Alike 4.0 License, which allows others to remix, transform, and build upon the work non-commercially, as long as the author is credited and the new creations are licensed under the identical terms.How to cite this article: Pablo Raul Devoto1, Federico Eduardo Minghinelli1, Juan José Mezzadri1, Derek Orlando Pipolo2, Matias Facundo Lacsi3, Pablo Gustavo Jalon1. Pedicle morphometry of the C7 and T1 vertebrae in an argentine population. 23-Aug-2024;15:295
How to cite this URL: Pablo Raul Devoto1, Federico Eduardo Minghinelli1, Juan José Mezzadri1, Derek Orlando Pipolo2, Matias Facundo Lacsi3, Pablo Gustavo Jalon1. Pedicle morphometry of the C7 and T1 vertebrae in an argentine population. 23-Aug-2024;15:295. Available from: https://surgicalneurologyint.com/?post_type=surgicalint_articles&p=13059
Abstract
Background: We evaluated how and whether the pedicular morphometry of the C7 and T1 vertebrae might impact C7/T1 spinal fusions for patients from Argentina.
Methods: Using computed tomography (CT) scans, we evaluated the pedicular morphology at the C7 and T1 levels.
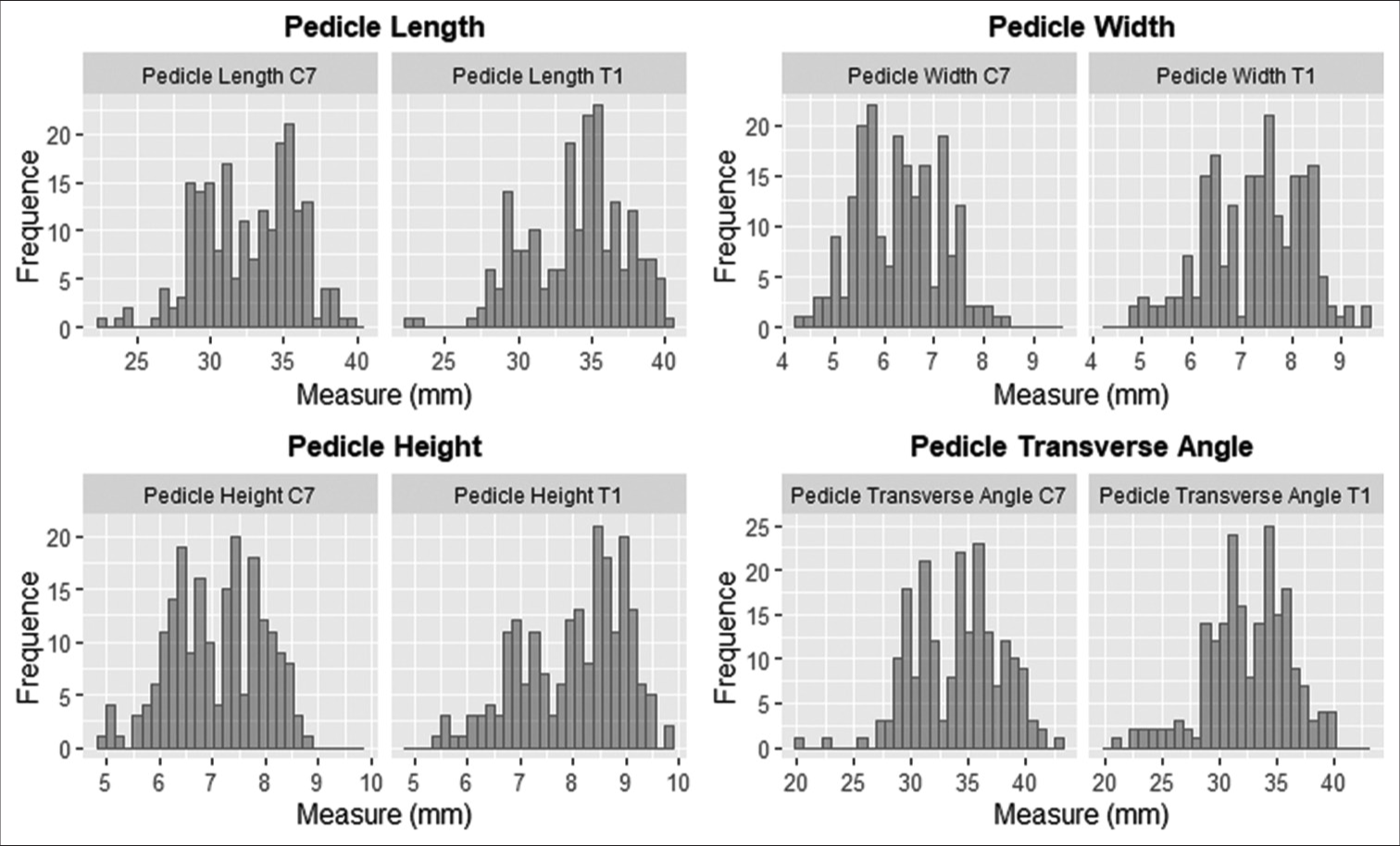
Results: Among 102 male and female CT studies, we observed significant differences in the height, width, length, and morphometry of the C7 and T1 pedicles.
Conclusion: This study of C7/T1 CT scans revealed significant sex-based morphometric differences, particularly in pedicle height, width, and length at C7 and T1. Given the notable variability in vertebral characteristics observed in our study sample, we recommend preoperative planning with CT scans for C7/T1 fusion.
Keywords: Argentine population, Cervicothoracic junction, Computed tomography, Pedicle morphometry, Transpedicular screws
INTRODUCTION
Performing C7/T1 fusions is crucial for treating various spinal pathologies. Notably, the C7 and T1 pedicles are relatively small and typically require pedicle screws.[
MATERIALS AND METHODS
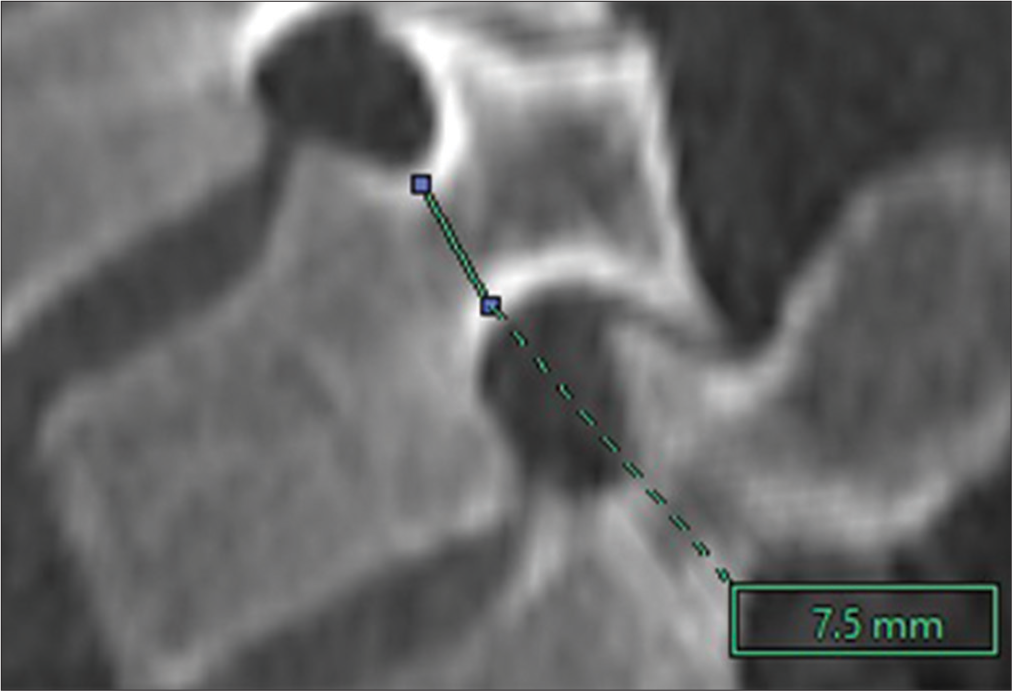
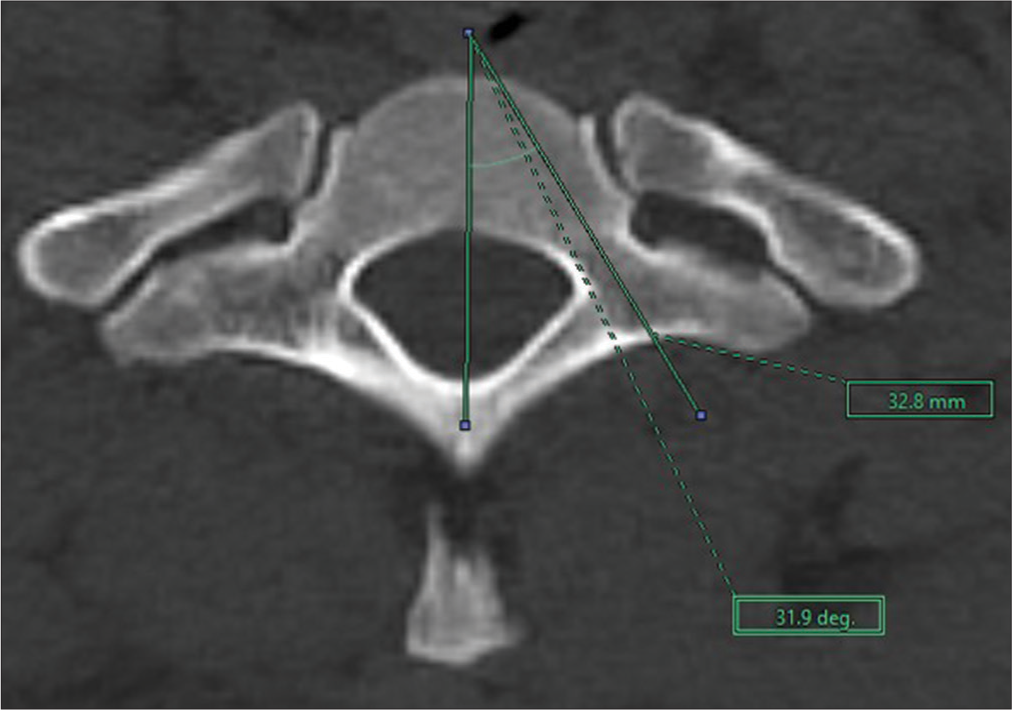
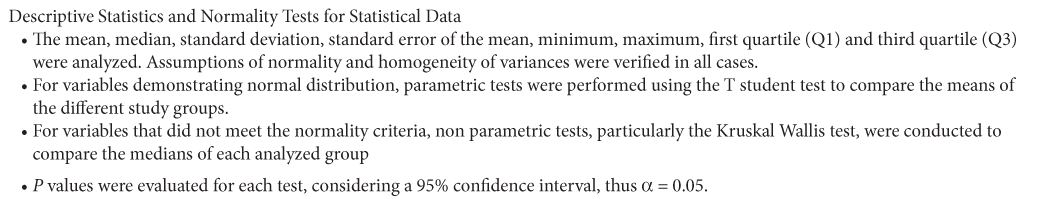
A retrospective cross-sectional study analyzing the C7/T1 pedicle morphology in adult computed tomography (CT) scans from male and female patients in Argentina between 2021 and 2022 was performed. The variables studied included age, C7–T1 pedicular laterality, pedicle width (PW), pedicle height (PH), pedicle axis length (PAL), and transverse angle [
RESULTS
A total of 102 CT scans (60 males and 42 females) were included in this study. Patient ages ranged from 23 to 69 years (mean 52). At both C7 and T1, males had greater PH, PW, and PAL compared to females [
DISCUSSION
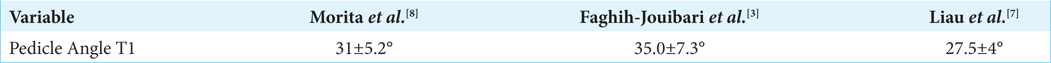
Many reports have studied the dimensions of C7 and T1 pedicles, which are relatively small and typically require 3.5– 4-mm diameter screws; considering this, larger screws may breach the pedicle wall. Here, we evaluated C7 and T1 PH, PW, and PAL based on 102 CT scans obtained in male and female patients from Argentina.[
The pedicle dimensions of certain patients in our sample were twice as large as those reported in the previous studies,[
Kotani et al.[
CONCLUSION
This study of C7/T1 CT scans revealed significant sex-based morphometric differences, particularly in PH, PW, and PAL at C7 and T1. Given the notable variability in vertebral characteristics observed in our study sample, we recommend preoperative planning with CT scans for C7/T1 fusion.
Ethical approval
The Institutional Review Board approval is not required.
Declaration of patient consent
The authors certify that they have obtained all appropriate patient consent.
Financial support and sponsorship
Nil.
Conflicts of interest
There are no conflicts of interest.
Use of artificial intelligence (AI)-assisted technology for manuscript preparation
The authors confirm that there was no use of artificial intelligence (AI)-assisted technology for assisting in the writing or editing of the manuscript and no images were manipulated using AI.
Disclaimer
The views and opinions expressed in this article are those of the authors and do not necessarily reflect the official policy or position of the Journal or its management. The information contained in this article should not be considered to be medical advice; patients should consult their own physicians for advice as to their specific medical needs.
References
1. Cho W, Eid AS, Chang UK. The use of pedicle screw-rod system for the posterior fixation in cervico-thoracic junction. J Korean Neurosurg Soc. 2010. 48: 46-52
2. Demiroz S, Erdem S. Computed tomography-based morphometric analysis of thoracic pedicles: An analysis of 1512 pedicles and their correlation with sex, age, weight and height. Turk Neurosurg. 2020. 30: 206-16
3. Faghih-Jouibari M, Moazzeni K, Amini-Navai A, Hanaei S, Abdollahzadeh S, Khanmohammadi R. Anatomical considerations for insertion of pedicular screw in cervicothoracic junction. Iran J Neurol. 2016. 15: 228-31
4. Herrero CF, Luis Do Nascimento A, Maranho DA, Ferreira-Filho NM, Nogueira CP, Nogueira-Barbosa MH. Cervical pedicle morphometry in a Latin American population. Medicine (United States). 2016. 95: e3947
5. Kotani Y, Cunningham BW, Abumi K, McAfee PC. Biomechanical analysis of cervical stabilization systems. An assessment of transpedicular screw fixation in the cervical spine. Spine. 1994. 19: 2529-39
6. Lee DH, Lee SW, Kang SJ, Hwang CJ, Kim NH, Bae JY. Optimal entry points and trajectories for cervical pedicle screw placement into subaxial cervical vertebrae. Eur Spine J. 2011. 20: 905-11
7. Liau KM, Yusof MI, Abdullah MS, Abdullah S, Yusof AH. Computed tomographic morphometry of thoracic pedicles: Safety margin of transpedicular screw fixation in Malaysian Malay population. Spine. 2006. 31: E545-50
8. Morita K, Ohashi H, Kawamura D, Tani S, Karagiozov K, Murayama Y. Thoracic and lumbar spine pedicle morphology in Japanese patients. Surg Radiol Anat. 2021. 43: 833-42
9. Munusamy T, Thien A, Anthony MG, Bakthavachalam R, Dinesh SK. Computed tomographic morphometric analysis of cervical pedicles in a multi-ethnic Asian population and relevance to subaxial cervical pedicle screw fixation. Eur Spine J. 2015. 24: 120-6
10. Onibokun A, Khoo LT, Bistazzoni S, Chen NF, Sassi M. Anatomical considerations for cervical pedicle screw insertion: The use of multiplanar computerized tomography measurements in 122 consecutive clinical cases. Spine J. 2009. 9: 729-34