- Department of Neurosurgery, Mito Saiseikai General Hospital, Mito, Japan
- Department of Neurosurgery, University of Tsukuba Hospital, Hitachi Social Cooperation Education Research Center/Hitachi General Hospital, Hitachi, Tsukuba, Japan
- Department of Neurosurgery, Graduate School of Comprehensive Human Sciences, University of Tsukuba, Tsukuba, Japan
- Department of Neurosugery, Ibaraki Seinan Iryo Center Hospital, Tsukuba, Japan
- Department of Neurosurgery, NHO Mito Medical Center, Tsukuba, Japan
- Department of Plastic Surgery, NHO Mito Medical Center, Tsukuba, Japan
- Department of Neurosurgery, Institute of Medicine, University of Tsukuba, Tsukuba, Japan
Correspondence Address:
Tomosato Yamazaki, Department of Neurosurgery, University of Tsukuba Hospital, Hitachi Social Cooperation Education Research Center/ Hitachi General Hospital, Hitachi, Japan.
DOI:10.25259/SNI_471_2024
Copyright: © 2024 Surgical Neurology International This is an open-access article distributed under the terms of the Creative Commons Attribution-Non Commercial-Share Alike 4.0 License, which allows others to remix, transform, and build upon the work non-commercially, as long as the author is credited and the new creations are licensed under the identical terms.How to cite this article: Yoshihiro Sato1, Tomosato Yamazaki2, Sho Hanai3, Daisuke Watanabe4, Noriyuki Kato5, Takehiro Kasai6, Alexander Zaboronok7, Eiichi Ishikawa7. Traumatic arteriovenous fistula of the superficial temporal artery caused by massive subcutaneous hematoma prompting surgical removal and endovascular treatment in a patient with neurofibromatosis type 1. 16-Aug-2024;15:289
How to cite this URL: Yoshihiro Sato1, Tomosato Yamazaki2, Sho Hanai3, Daisuke Watanabe4, Noriyuki Kato5, Takehiro Kasai6, Alexander Zaboronok7, Eiichi Ishikawa7. Traumatic arteriovenous fistula of the superficial temporal artery caused by massive subcutaneous hematoma prompting surgical removal and endovascular treatment in a patient with neurofibromatosis type 1. 16-Aug-2024;15:289. Available from: https://surgicalneurologyint.com/surgicalint-articles/13042/
Abstract
Background: Neurofibromatosis type 1 (NF-1) is often characterized by vascular disorders related to vessel vulnerability that can lead to unfavorable outcomes. Here, we describe a case of NF-1 complicated with a massive subcutaneous hematoma posing a risk of visual impairment for which rapid decompression and a subsequent less invasive approach result in a favorable outcome.
Case Description: A 40-year-old woman with NF-1 presented with a massive left subcutaneous temporal hematoma following a mild head contusion. Four days after hospitalization, the hematoma increased in size and severely compressed the left eye, prompting immediate hematoma removal to preserve visual function. Immediately after the hematoma removal, a superficial temporal arteriovenous fistula was found on the digital subtraction angiography and embolized by the endovascular procedure. Her visual acuity was preserved, and no bleeding recurrence was observed throughout the follow-up.
Conclusion: Surgical hematoma removal followed by endovascular treatment was effective in preserving visual function. Since vessel fragility is characteristic of patients with NF-1, it should be kept in mind that vascular complications may lead to serious clinical outcomes. In certain NF-1 cases, less invasive treatments for vascular abnormalities may be preferable.
Keywords: Endovascular treatment, Neurofibromatosis type 1, Subcutaneous hematoma, Superficial temporal artery, Traumatic arteriovenous fistula
INTRODUCTION
Neurofibromatosis type 1 (NF-1) is an autosomal dominant disease occurring in 1 of 3000–4000 individuals with characteristic manifestations of café-au-lait spots, neurofibromas, and Lisch nodules.[
CASE REPORT
A 40-year-old woman with NF-1 with a history of optic pathway/hypothalamic glioma underwent surgery with the right eye removal at the age of 3. She recently hit her left temple slightly on the corner of a PC monitor. Three days later, that area suddenly swelled, and she visited our hospital. She was alert without a neurological deficit. Head computed tomography (CT) showed a marked subcutaneous hematoma on the left [
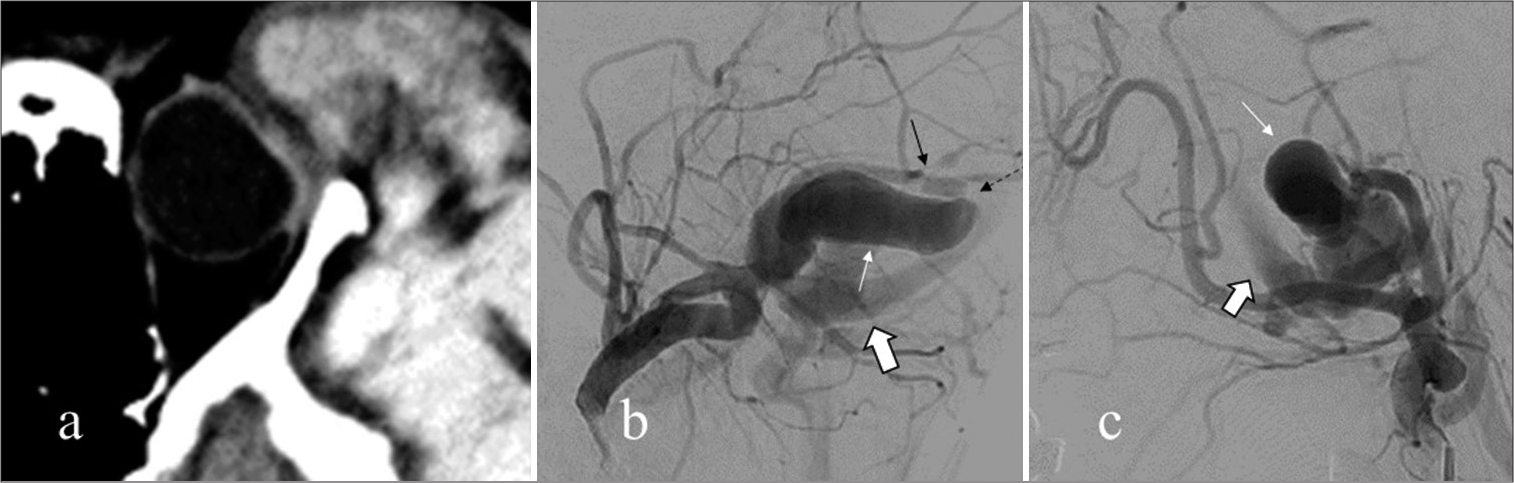
Figure 1:
(a) Head CT: a massive left subcutaneous hematoma on admission. (b) AP and (c) lateral views of the early arterial phase external carotid artery (ECA) digital subtraction angiography (DSA): poorly contrasted distal left STA due to compression by hematoma (black arrow). (d) The lateral view of the late arterial phase ECA DSA: minor extravasation near the contusion site (white arrow).
Four days after admission, the hematoma suddenly enlarged, preventing the patient from opening her left eye, and intraocular pressure increased to the point of causing blindness. Head CT revealed left eye deformation due to compression by the enlarging hematoma [
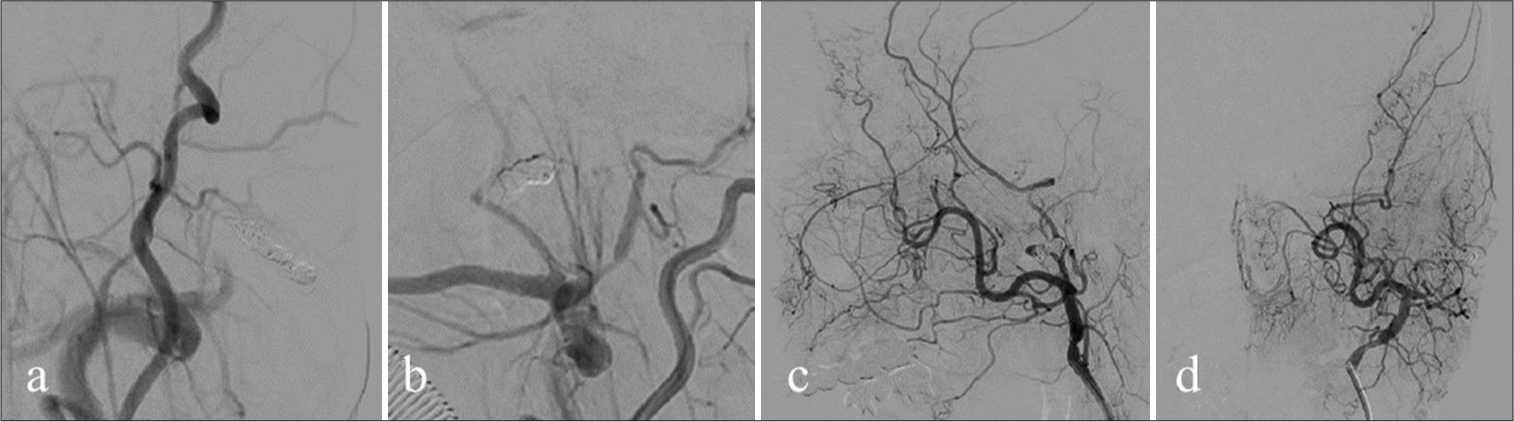
Figure 2:
(a) Axial computed tomography. (b) Anterior- posterior view of the left external carotid artery (ECA) digital subtraction angiography (DSA): string sign of the left STA (black arrow), the dilated vein (white arrows), and the vein (bold arrows) draining via the arteriovenous fistula (dotted arrow). (c) Lateral view of the left ECA DSA: the dilated vein (white arrows) and the vein (bold arrows) draining via the arteriovenous fistula.
DISCUSSION
We treated a patient with NF-1 effectively using a combination of surgical decompression and endovascular treatment. In NF-1, hemorrhagic complications may be associated with vessel vulnerability. Mild injuries can lead to unfavorable outcomes, such as a life-threatening brachial artery hemorrhage requiring amputation of the upper extremity[
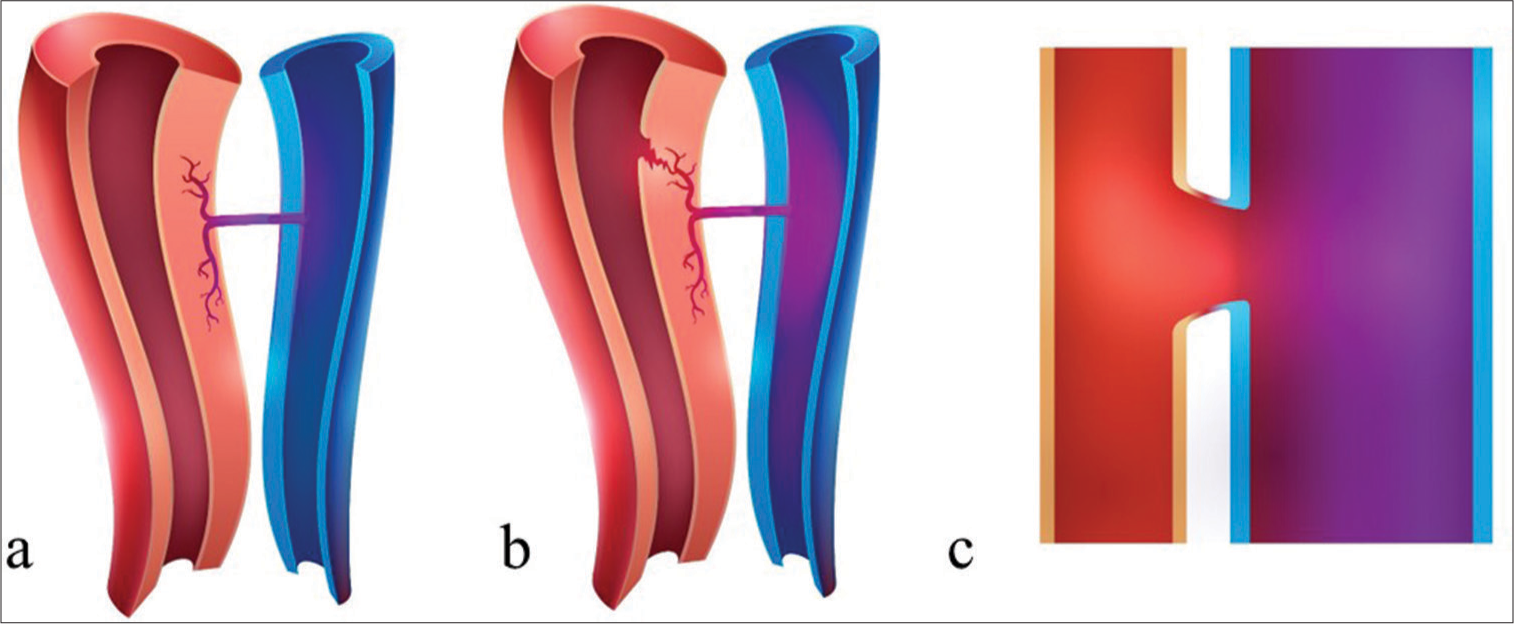
The laceration theory has been proposed as a mechanism of traumatic AVF formation.[
In NF-1, attention should be paid to vessel vulnerability, which can lead to serious consequences. Our case may be instructive in terms of hemorrhagic complications, where emergent and less invasive interventions proved favorable.
CONCLUSION
We report a case of a massive subcutaneous hemorrhage that caused STA AVF formation in a patient with NF-1. Surgical hematoma removal followed by endovascular treatment was effective in preserving visual function. Since vessel fragility is characteristic of patients with NF-1, it should be kept in mind that vascular complications may lead to serious clinical outcomes. In certain NF-1 cases, less invasive treatment of vascular abnormalities might be favorable.
Ethical approval
The Institutional Review Board approval is not required.
Declaration of patient consent
The authors certify that they have obtained all appropriate patient consent.
Financial support and sponsorship
Nil.
Conflicts of interest
There are no conflicts of interest.
Use of artificial intelligence (AI)-assisted technology for manuscript preparation
The authors confirm that there was no use of artificial intelligence (AI)-assisted technology for assisting in the writing or editing of the manuscript and no images were manipulated using AI.
Disclaimer
The views and opinions expressed in this article are those of the authors and do not necessarily reflect the official policy or position of the Journal or its management. The information contained in this article should not be considered to be medical advice; patients should consult their own physicians for advice as to their specific medical needs.
Acknowledgment
The authors would like to thank Dr. Jaejeong Kim for creating the illustrations in Figure 4.
References
1. Bhaskar S, Sobti S, Singh AK. Massive scalp hematoma due to diffuse neurofibroma in NF-1. Clin Neurol Neurosurg. 2013. 115: 477-8
2. Biegaj E, Rutkowska-Zimirska J, Radzymińska-Maliszewska M, Zaremba A, Pniewski J. Arteriovenous fistula of superficial temporal vessels. Folia Morphol (Warsz). 2019. 78: 879-82
3. Chew DK, Muto PM, Gordon JK, Straceski AJ, Donaldson MC. Spontaneous aortic dissection and rupture in a patient with neurofibromatosis. J Vasc Surg. 2001. 34: 364-6
4. Evans DG, Howard E, Giblin C, Clancy T, Spencer H, Huson SM. Birth incidence and prevalence of tumor-prone syndromes: estimates from a UK family genetic register service. Am J Med Genet A. 2010. 152A: 327-32
5. Gössl M, Rosol M, Malyar NM, Fitzpatrick LA, Beighley PE, Zamir M. Functional anatomy and hemodynamic characteristics of vasa vasorum in the walls of porcine coronary arteries. Anat Rec Part A. 2003. 272A: 526-37
6. Greene JF, Fitzwater JE, Burgess J. Arterial lesions associated with neurofibromatosis. Am J Clin Pathol. 1974. 62: 481-7
7. Iwama T, Mizutani K, Kubo H, Katsumata M, Akiyama T, Toda M. A case of neurofibromatosis type 1 diagnosed after idiopathic rupture of superficial temporal artery pseudoaneurysm requiring endovascular treatment. NMC Case Rep J. 2023. 10: 125-30
8. Lee J, Kim Y. Life-threatening brachial artery hemorrhage and a lethal outcome in patients with neurofibromatosis type 1: Two case reports and a review of the literature. J Int Med Res. 2021. 49: 03000605211025344
9. Li F, Zhu S, Liu Y, Chen Y, Chi L, Chen G. Traumatic arteriovenous fistula of the superficial temporal artery. J Clin Neurosci. 2007. 14: 595-600
10. Negreira KE, Lichtenberger JP, Allais B, Alhaddad A, Bernetich M, Jain V. Subclavian artery branch pseudoaneurysm rupture with massive hemothorax in a patient with neurofibromatosis type 1. Chest. 2020. 157: e103-5
11. Raborn J, McCafferty BJ, Gunn AJ, Moawad S, Mahmoud K, Abdel AA. Endovascular management of neurofibromatosis type I-associated vasculopathy: A case series and brief review of the literature. Vasc Endovascular Surg. 2020. 54: 182-90
12. Shoenenberger F, Mueller A. On the vascularization of the bovine aortic wall. Halvet Physiol Pharmacol Acta. 1960. 18: 13650